General Dentistry in Canterbury
Wear your best smile with the help of our talented team.
With our personal approach to general dentistry, Dentistry in Canterbury transforms your regular dental check-ups into a fun, relaxed and fulfilling experience. Our team delivers high-end general dental services, such as teeth cleaning and gum disease treatments, at the highest quality.
All patients are welcome to our clinic. Whether you need to pop in to fix a problem tooth or book a regular check-up on behalf of your family, don’t hesitate to contact Dentistry in Canterbury today and achieve your smile goals.

CHOOSE DENTISTRY IN CANTERBURY
For a personal touch
NEW TO DENTISTRY IN CANTERBURY? DISCOVER OUR IDEOLOGY OF CARE
Team
Award-winning Canterbury Dentists

Dr. Julie Ghaly
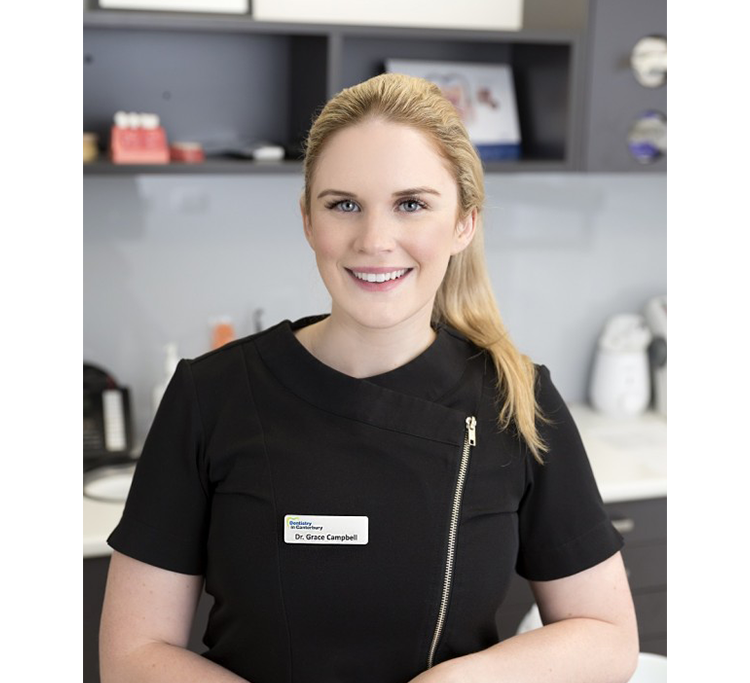
Dr. Grace Campbell

Dr. Claire Abraham

Dr. Jessica Attalla

Dr. Marina Attalla
Dr. Angelos Sourial

Dr. Gina Malak

Dr. Marianne Chua

Dr. Teodora Litovska
Dr. Amisha Hindocha

Alanna Grieger

Radhika Arasu

Ying Mu

Dr. Julie Ghaly
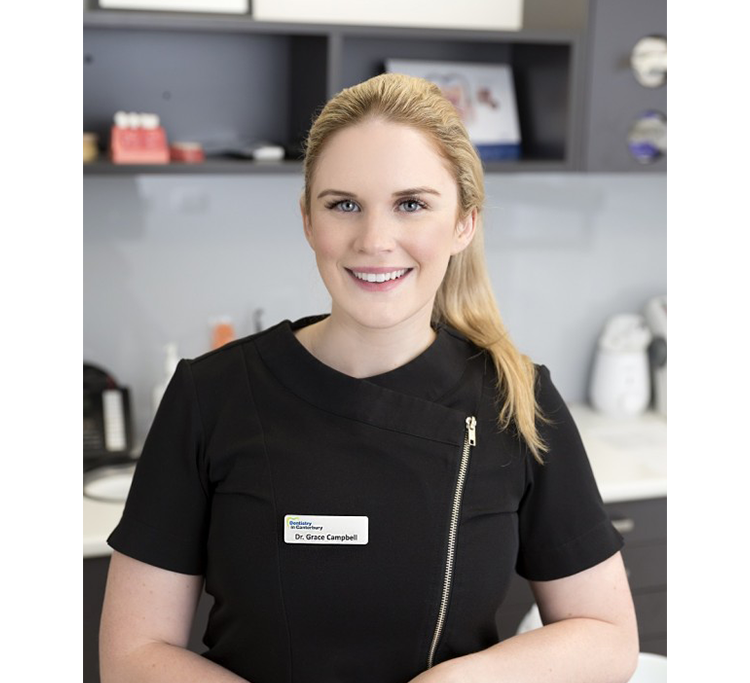
Dr. Grace Campbell

Dr. Claire Abraham

Dr. Jessica Attalla

Dr. Marina Attalla

Dr. Mark Farag

Alanna Grieger

Elizabeth Wells

Radhika Arasu
A warm, welcoming service
The care and comfort of our patients is our main priority.State-of-the-art technology
We use cutting edge equipment & the latest technology.Calm, soothing environment
Ensuring your visit is as comfortable and pain-free as possible.Family-owned & trusted for over 35 years
Expect the highest standards of care from our friendly, experienced team.General dentistry is for patients of all ages offering complete, comprehensive dental health care.
Learn More NowWe work toward creating youthful smiles for patients whose natural teeth require replacement.
Learn More NowGeneral dentistry is for patients of all ages offering complete, comprehensive dental health care.
Learn More NowWe work toward creating youthful smiles for patients whose natural teeth require replacement.
Learn More NowQuality dental care, whatever your needs
We strive to provide the highest level of dental care for all age groups. Our general services include preventative care, restorative dentistry and family dental therapy, covering everything from fillings to veneers.
Across all treatments, our team are leading experts. Beyond their dental expertise, they are warm, friendly people, capable of putting even the most anxious minds at ease. With their support, you’ll learn the core principles of good oral hygiene to maintain your teeth for life and develop your dream smile.
The importance of general dental care
Regular visits to the dentist are key to overall physical health. If you’re due for a regular dental check-up or have a concern, book an appointment at your earliest convenience.
Neglecting your teeth could lead to tooth or gum disease as well as permanent structural damage. An examination from a leading Melbourne clinic like Dentistry in Canterbury will help put your mind at rest and resolve any issue before they develop further.


















At Dentistry in Canterbury we excel at providing high quality comprehensive general dental treatment. We also specialise in anti-aging and facial enhancement treatments. Our team has a gentle and friendly manner.
Copyright © 2022 | Dentistry In Canterbury ABN: 24 985 368 567 | Ts & Cs | Privacy Policy
